Beginning a successful exercise regimen requires an understanding of how to avoid injury and ensure you are properly prepared for the increased stress that this will play on your body. To take the stress out of your work out, this article will showcase why the engines of locomotion are firmly planted on the ground and why they are so important.
Foot and Ankle Anatomy
The human foot is a complex machine consisting of a flexible network of structures including: bones, joints, muscles, tendons and ligaments. Each foot consists of 26 bones, 30 joints and more than 100 muscles/tendons/ligaments all of which work together to provide support, balance and mobility. Sections of the foot are divided into three recognized areas:
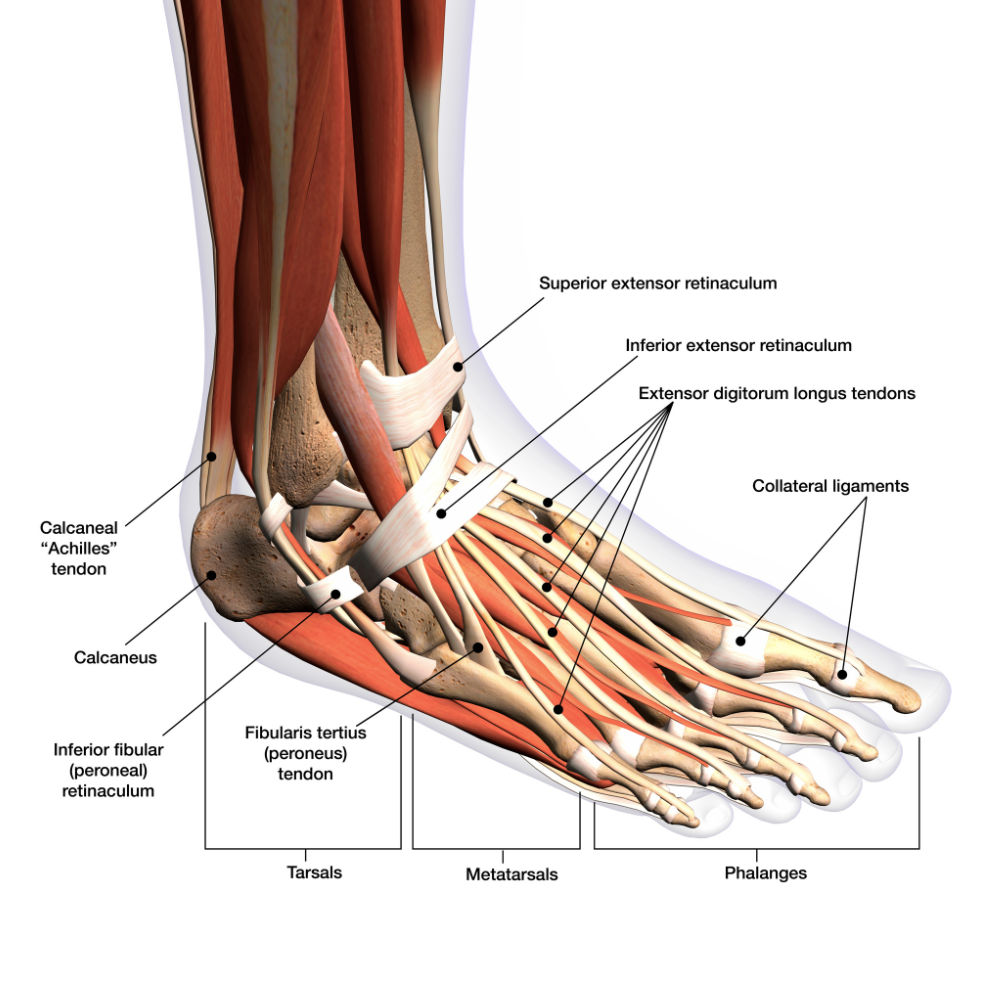
- The Forefoot: includes the bones of your toes (phalanges) and the five longer bones that attach to them, called metatarsals.
- The Midfoot: consists of a puzzle-like pyramid of bones that contribute to the arches of the feet. These include three cuneiform bones (meaning wedge-shaped), the cuboid bone (square) and the navicular bone which gets its name from being boat-shaped.
- The Hindfoot: contains structures to form the heel and ankle. The talus bone supports the bones of the lower leg (fibula and tibia) to create the ankle. The calcaneus (heel bone) is the largest bone in the foot.
What many people don’t realize is that each foot also contains three arches, not just one. When functioning properly, they work the same way as a spring, allowing the feet to bear the weight of the body and absorb the shock produced during activities like walking, running and jumping.
- The Medial Longitudinal Arch: Stretches from the ball of the foot (under the big toe) to the heel. This is what most people think of when discussing ‘the arch of the foot’ because it is the highest and most noticeable arch.
- The Lateral Longitudinal Arch: Spans from the ‘ball’ under the pinky toe to the heel. Note that what we think of as the balls of our feet are actually the heads of the metatarsal long bones where they meet the toes.
- The Anterior Transverse Arch: Crosses the width of the foot from the ball of the foot under the big toe to the ‘ball’ under the pinky toe and represents the arc of the metatarsal heads.
All of these structures form an association of moveable parts that work synergistically. As experts in optimizing joint function and alignment, doctors of chiropractic (DCs) not only address joints in the spine, they also work with the many joints of the upper and lower extremities and have a detailed understanding of the complexities of the foot and its many supporting structures.
Understanding the Kinetic Chain
Feet are the body’s foundation. Our feet provide the groundwork for our upright weight-bearing posture. This makes them a primary influence when we talk about the kinetic chain in the body. ‘Kinetic chain’ is actually an engineering concept used to describe human movement. It refers to the interconnectedness of the body and how our body areas work together, compensate for or affect one another to perform movements. When choosing footwear, the importance of having proper support to promote functional stability for the many joints and arches of the feet cannot be undervalued.
It has been estimated that every pound of body weight exerts up to three pounds of force that the feet have to absorb when walking. If a person weighs 200 lbs., the force on the feet will be up to 600 lbs. When running, that number grows exponentially with up to seven pounds of force per pound of body weight being exerted which would translate to 1,400 pounds of pressure per footfall for our 200 lb. example.
Foot and ankle biomechanics influence motion and function throughout our skeletal structure. Improper gait, foot strike or subtle differences in functionality from one foot to the other can all translate stresses up through the knees and into the hips, pelvis and spine. Anyone who has ever broken a toe, been in a leg cast or sprained an ankle will inherently relate to this concept of how a change in gait can cause pain in other areas. However, an injury does not have to be the primary cause of compensatory pain. Pain can also manifest simply from the way you are walking.
Watching your Step
Over-pronation, for example, is a very common finding in patients. It means you are walking more on the inside arch of your foot. Walking this way actually creates an unnatural internal rotation in the lower leg, which when combined with typical joint positions needed to simply walk, translates to stress in the knee joint and has been shown to increase the risk for knee injuries and back pain.
Internal rotation of the lower leg from over-pronation has also been correlated with an increased Q-angle (Q for quadriceps). The Q-angle is a valuable indicator when evaluating biomechanical function in the lower extremity. The assessment of it provides useful information about the alignment of the hips, pelvis, leg and foot. Increased Q-angle measurements have been associated with higher incidence of ACL injuries.
As we continue up the body, we find multiple studies have also linked over-pronation in the foot to unspecified low back pain. In 2017, a randomized controlled trial was published in the journal Archives of Physical Medicine and Rehabilitation which concluded that over 40% of patient participants had a significant reduction in low back pain and an increase in function with a combination of custom foot orthotics and chiropractic care. This exemplifies how much impact a well-functioning foundation can have on our musculoskeletal system as a whole.
Optimum Foot Strike and Support
The way you walk contributes to significant outcomes. Years of improper walking can lead to joint stress, pain, degeneration, spurs, fallen arches, and in the shorter term, can translate to compensation and resulting pain in your ankles, knees, hips and spine.
Most people will demonstrate a better foot strike when barefoot. This is because the nerves in your feet can feel the ground and adjust the way your steps hit the floor. Being barefoot on the beach isn’t just a daydream, it also takes more effort than walking on a hard surface and strengthens your foot and ankle while you burn more calories!
With shoes, people are more prone to developing bad walking habits such as dragging the feet, heavy impact steps and limiting natural movement in the joints of the foot. Most of us, however, need to wear shoes the majority of our waking hours. Watch the soles of your shoes, if the outer sole wears down unevenly it can be a strong clue that you need to adjust your foot strike/gait.
To best support your feet, keep the following considerations in mind to help optimize the way that you walk:
- Proper Posture: Stand up straight/shoulders back/head supported by your spine. Do not look down (such as at your feet or your phone), look forward. Feet should be shoulder width apart/chest forward and abdominals/core muscles engaged.
- Foot Strike: Should begin with the heel landing squarely on the floor. As you roll onto the entire ball of your foot the heel should begin to slightly lift and toes should be flexed. The step should spread to each toe, beginning with the small toe hitting the floor and lifting up off the ground as you complete the step. Mindfully watch to see if your step has you rolling inward or outward.
- Gait: Ensure your toes face forward to keep the ankles in a neutral position. If toes are in a ‘V’ outward or inward it creates strain on soft tissues of the ankle and heel.
- Shoe Fit: Ensure that your shoes are supportive for all areas of the foot and that they are flexible and provide ample width. Also note if they are causing blisters. Custom orthotics may be indicated for many patients that require extra support to ensure that foot strike is optimized.
Urban exercise myths like ‘no pain, no gain’ certainly do not apply to the foot. Your feet should not feel pain during normal walking or with exercise activities. In the chiropractic office, DCs can analyze and advise on your foot strike/gait, evaluate the complexities of the foot and kinetic chain, adjust affected areas to optimize joint function and mobility, offer strengthening exercises and many offices are also equipped to take foot molds and have custom orthotics created for patients that need to augment foot support.
For more information on the benefits of walking and running read the Next Step Walking Guide and tune into our ‘Adjusted Reality’ podcast interview with elite endurance athlete, author and adventurer, Colin O’Brady, as he discusses the benefits of walking and how shifts in mindset can enhance our time on the trail.